Unit 2 Biology (1st Year CSE)
PDF of All Lectures
Lectures 1 Transcript
Sources of Biomedical Signals
Biomedical signals/physiological signals are those signals (phenomenon that conveys information) which are used primarily for extracting information on a biological system under investigation. Our body produces various physiological signals. The accessibility to these signals is important because these signals:
Can be internal (Blood pressure)
May emanate from the body (infrared radiation)
Maybe derived from tissue sample (Blood or tissue biopsy)
All physiological signals can grouped as:
Bio potential
Pressure
Flow
Dimensions (imaging)
Displacement (velocity, force, acceleration)
Impendence
Temperature
Chemical concentration and composition
A transducer converts a physical signal into an electrical output. A transducer should only respond to the targeted form of energy existing in the physiological signal and it must exclude all other energies. It should also interface with the living system in such a way that it extracts minimum energy and it should not be invasive.
Biomedical Signals are classified as follows:
Bioelectric signals: These signals are generated by the nerve and muscle cells. Their basic source is the cell membrane which under certain conditions maybe excited to generate an action potential. The electric field generated by the action of many cells constitutes the bioelectric signal. The most common examples of bioelectric signals are the ECG (Electrocardiographic) and EEG (Electroencephalographic) signals. (Link to amazon products for ECG and EEG)
Biomechanical signals: These signals are generated due to some mechanical function of a physiological system. They include all types of motion and displacement signals, pressure, flow signals etc. in the physiological system. The respiratory physiological system performs its function by the chest movement. This movement can be measure and analysed.
Biocoustic signals: These signals are created by the physiological system in which either flow of blood or air takes place. The flow of the blood in the heart as well as inspiration and expiration of the lungs takes place accompanied with unique acoustic signals.
Bio-impedance signals: The impedance of the skin depends upon; the composition of the skin, blood distribution and blood volume through the skin. The measurement of impedance helps in finding the state of skin and functioning of various physiological systems. The voltage drop due to the tissue impedance is a bio-impedance signal.
Biochemical signal: The signals which are obtained as a result of chemical measurements from the living tissue or from samples analysed in the laboratory. The examples of these include; measurement of partial pressure of carbon-dioxide (pCO2), partial pressure of oxygen (pO2) and concentration of various ions in the blood.
Bio-optical signals: These signals are produced by the optical variation by the functioning of the physiological system. The blood oxygenation can be determined by measuring transmitted and reflected light occurring from the blood vessel.
Biomagnetic signals: Extremely weak magnetic fields are produced by various organs such as the brain, heart and lungs. The measurement of these signals provides information which is not available in other types of bio-signals such as bioelectric signals. A typical example is the Magnetoencephalography which is obtained by recording the biomagnetic signals from the brain
What is Biomedical Instrumentation?
Biomedical instrumentation and engineering is the application of knowledge and technologies to solve problems related to living biological systems. It involves diagnosis, treatment and prevention of disease in human. As the medical field is emerging, the area of Biomedical Engineering is an expanding field. We use the term “bio” to denote something related to life. When basics of physics and chemistry get applied to the living things, and we name them as Biophysics and Biochemistry. So when the discipline of engineering and medicine interacts, it is called Biomedical Engineering.
It involves measurement of biological signals like ECG, EMG, or any electrical signals generated in the human body. Biomedical Instrumentation helps physicians to diagnose the problem and provide treatment. To measure biological signals and to design a medical instrument, concepts of electronics and measurement techniques are needed.
Components of Biomedical Instrumentation System
Any medical instrument consists of the following functional basic parts:
1. Measurand: The measurand is the physical quantity, and the instrumentation systems measure it. Human body acts as the source for measurand, and it generates bio-signals. Example: body surface or blood pressure in the heart
2. Sensor / Transducer: The transducer converts one form of energy to another form usually electrical energy. For example, the piezoelectric signal which converts mechanical vibrations into the electrical signal.
The transducer produces a usable output depending on the measurand. The sensor is used to sense the signal from the source. It is used to interface the signal with the human.
3. Signal Conditioner: Signal conditioning circuits are used to convert the output from the transducer into an electrical value. The instrument system sends this quantity to the display or recording system. Generally, signal conditioning process includes amplification, filtering, analogue to digital and Digital to analogue conversions. Signal conditioning improves the sensitivity of instruments.
4. Display: It is used to provide a visual representation of the measured parameter or quantity. Example: Chart recorder, Cathode Ray oscilloscope (CRO). Sometimes alarms are used to hear the audio signals. Example: Signals generated in Doppler Ultrasound Scanner used for Fetal Monitoring.
5. Data Storage and Data Transmission: Data storage is used to store the data and can be used for future reference. Recent days Electronic Health records are utilized in hospitals. Data transmission is used in Telemetric systems, where data can be transmitted from one location to another remotely.
Key Performance Requirements of Effective Biomedical Instrumentation Systems
The information obtained from a medical sensor or transducer is usually in form of current intensity, voltage level, frequency or signal phase relative to a standard.
We look at some of the performance requirements considered in biomedical instrumentation systems as discussed below:
To make accurate measurements of voltage, it is necessary to have the input impedance of the measuring device larger than the output impedance of the signal source. This is to minimize the error that would occur if an appreciable fraction of the signal source were dropped across the source impedance.
An accurate measurement of current source signals requires that the source output impedance be larger than receiver input impedance. In an ideal situation, a receiver that exhibits zero input impedance would not cause any disturbance to the current source. Hence, high-impedance current sources are more easily handled than low-impedance current sources.
Generally, the frequency response of the system should be compatible with the operating range of the signal being measured. To process the signal waveform without distortion, the bandpass of the system must include all of the frequency components of the signal that contribute significantly to the signal strength. The range can be determined quantitatively by obtaining a Fourier analysis of the signal.
Electrical signals are usually affected by spurious signals components or noise. Biomedical instruments are designed in such a way that the noise is minimized to enable accurate and sensitive measurement. To extract information from noisy signals, it is necessary to enhance signal-to-noise ratio. Using techniques like bandwidth reduction.
Digital processing is preferred over analog processing. Digital techniques are advantageous over analog techniques e.g. they are not affected by temperature that affects analog devices. The digital devices have a powerful performance since they are able to implement complex algorithms.
Lecture 2 Transcript
LECTURE NOTES- 2
Microprocessors in Medical instruments
1. Patient Monitoring in Intensive Care Unit.
2. Pathological Analysis and the measurement of parameters like blood pressure and temperature.
3. Measurement of heart activity.
4. Ultrasound Processing unit.
5. MRI scanning
6. CT scanning etc.
PC base medical Instruments
The days of enormous computers and huge medical devices are nearly over — as technology advances, it shrinks, and in no field is that more useful than in healthcare. Smaller tech means more mobile and agile medical services, which in turn means more options for patients and providers alike.
Tablets fill this role nicely — they’re thin, sleek, touchscreen, and the right tablet has decent power, too. However, there are some pitfalls to avoid. While an iPad may be a familiar platform for many users, Apple’s hardware and software is propriety and a closed environment. Guarantees of compatibility are slim, and chances of customization nil.
On the other hand, a medical tablet that can run PC software is going to play nice with most apps and programs designed for medical use, and can more easily talk to and interface with existing desktops and laptops. Plus, over 79% of clinicians are already familiar with tablets and make use of them daily, so training time is decreased.
The following medical devices, and their manufacturers, can all benefit from the addition of a tough, compact, purpose-built medical grade tablet.
1. Physical Therapy Devices
Physical therapy is an already exhausting experience, but it can be improved with the use of the latest technology. A readily available medical tablet in a therapy room can provide both patient and clinician with useful resources like instruction videos and therapy logs. As a bonus, these tablets can also be used for telehealth and at-home PT.
Apps like PT Pal Pro and Pain Therapy allow both parties to keep in touch, for the physical therapist to suggest and send exercises, and for the patient to be guided correctly through each motion.
An embedded medical tablet can also be used to power the programming behind physical therapy machines. Rehabilitation robots are designed to use their arms to help patients make perfectly repeatable, precision movements that even an expert physical therapist would be unable to match.
The robot’s perfect ability to guide a patient through an exercise requires an integrated tablet with both power, durability, and portability – these robots are all about movement, and having them plugged in and unmoving just doesn’t work.
2. Medical Imaging Machines
Medical imaging is evolving, expanding, through the use of cutting-edge techniques like ghost imaging, portable ultrasound, and advanced AI analysis. Of course, imaging machines like MRI, Xray, O-Arm, and others require an integrated computer to function at all. Both of these factors are creating a demand for medical computers that can plug-and-play into medical devices without a lot of hassle or compatibility issues.
A high-definition 4k medical computer or medical monitor provides the kind of clear, full-color imaging required to take detailed pictures and video, and it does so without sacrificing durability and the longevity required by modern medical budgets.
Tablets and battery-powered medical all-in-one PCs also provide a huge boon to mobile imaging applications like dental, gynecological, or radiological trucks, either for rural or urban use. Since battery-powered medical tablets, monitors, and panel PCs often have redundant battery bays and a long time between charge cycles, they can run imaging machines with no problem for great lengths of time without going near a power socket.
Telepresence Robots
A telepresence robot is a new concept that has been cleared by the FDA and may start appearing in more healthcare facilities soon. They’re designed to provide some telehealth relief to patients and crowded healthcare providers alike. With a known shortage of doctors and nurses, it’s time to explore alternatives to keeping patient care at its highest levels.
Controlled by both an embedded medical tablet and a distant tablet or medical computer, telepresence robots are designed to give patients facetime when they might otherwise have been waiting for treatment. Doctors can diagnose and treat patients via the use of these robots, though they are most often used for remote consultations with distant specialists. It can save the specialist a long car, train, or plane trip, while at the same time getting the ball rolling on the patient’s healthcare plan in the meantime.
These medical devices can obviously benefit from integrated medical computers. Instead of a consumer model of tablet or other computer, the telepresence robot can maintain its IP65 and 60601 rating with minimal effort by using a medical tablet for long-distance communication.
4. Robot-Assisted Surgical Systems
Nearly two decades ago, the FDA approved the use of the da Vinci Surgical System, a massive surgical robotic suite that surgeons use today to fine-tune their incisions for greater patient care.
Traditional surgery has relied on steady hands and proper instrumentation, but with systems like these, patients have seen a drop in significant problems. Using sophisticated controls and a surgical monitor that magnifies the surgical site, doctors can manipulate several arms above the patient that can carefully incise and stitch up areas of the body. The result is reduced blood loss, shorter recovery times, and fewer health complications. It’s great for cosmetic reasons too — surgical scars are less apparent because the arms create tiny holes instead of large incisions.
These systems, and others like them, require top, medical grade panel PCs or medical monitors that can be integrated within the machine itself. And since the robot-assisted surgery equipment goes inside the operating theatre, it must conform to stringent guidelines. A medical grade panel PC can be integrated easily, and its antimicrobial case and fanless design fit all the IEC/EN/UL60601-1 requirements needed to work safely near patients and in surgical environments.
Meeting Medical Requirements
Medical devices and medical computers make for excellent partners — why reinvent the wheel in having to design a PC around an existing device, and why deal with the failures of consumer-level computers and less-regulated standards.
Visit Cybernet today to learn more about how to integrate medical tablets and medical computers into any existing medical device.
Lecture 4 Transcript
Lecture 4
31 Measurement Input Sources
Desired Inputs: Measurands that the instrument is designed to isolate.
Interfering Inputs: Quantities that accidentally affect the instrument as a consequence of the principles used to acquire and process the desired inputs.
Modifying Inputs: Quantities that cause a change in the input –output relations of the instrument.
32 Example: ECG Signal Measurement
Desired Input: ECG voltage (Vecg)
Interfering Input: 60/50 Hz noise voltage, displacement currents
Modifying Input: – orientation of the patient cables when the plane of the cable is perpendicular to the magnetic field the magnetic interference is maximal
Figure: Simplified electrocardiographic recording system Two possible interfering inputs are stray magnetic fields and capacitive coupled noise. Orientation of patient cables and changes in electrode–skin impedance are two possible modifying inputs. Z1 and Z2 represent the electrode–skin interface impedances.
33 Characteristics of Instrument Performance
Evaluate new instrument designs, quantitative criteria for the performance of instruments.
These criteria must clearly specify how well an instrument measures the desired input and how much the output depends on interfering and modifying inputs.
Characteristics of instrument performance are usually subdivided into two classes on the basis of the frequency of the input signals.
Static Characteristics
Dynamic Characteristics
Static Characteristics describe the performance of instruments for dc or very low frequency inputs.
The output for a wide range of constant inputs demonstrate the quality of the measurement, including nonlinear and statistical effects.
Dynamic Characteristics require the use of differential and/or integral equations to describe the quality of the measurements.
35 Generalized Static Characteristics
Following are the parameters used to evaluate medical instrument:
Accuracy: refers to the degree of conformity between the measurand and the standard. It can be calculated using the difference between the true value and the measured value divided by the true value.
Resolution: It refers to the degree to which the measurand can be broken into identifiable adjacent parts.
Reproducibility: The ability of an instrument to give the same output for equal inputs applied over some period of time.
Statistical Control: It ensures ensures that random variations in measured quantities that result from all factors that influence the measurement process is tolerable.
Static Sensitivity: Static Sensitivity of instrument or system is the ratio of the incremental output quantity to the incremental input quantity.
Zero Drift: It occurs when all the output values increase or decrease by the same absolute amount.
Factors can cause zero drift: manufacturing misalignment, variations in ambient temperature, hysteresis, vibration, shock, and sensitivity to forces from undesired directions.
Linearity: A system or element is linear if it has properties such that if y1=x1 and y2=x2, then y1+y2 is the response to x1+x2, and Ky1=Kx1. They are clearly satisfied for an instrument with a calibration
curve that is a straight line.
38 Input Ranges: The normal linear operating range specifies the maximal or near maximal inputs that give linear outputs.
Input Impedance: It is the ratio of the phasor equivalent of a steady-state sinusoidal effort input variable (voltage, force, pressure) to the phasor equivalent of a steady-state sinusoidal flow input
variable (current, velocity, flow).
39 Generalized Dynamic Characteristics
Most of the biological signals time-varying in nature and therefore we should make sure that the instrument is a time-invariant system for an accurate measurement.
The dynamic characteristics of an instrument include its transfer function, its frequency response, and its phase or time delay.
Dynamic characteristics require the use of differential or integral equations to describe the quality of the measurements.
Transfer functions are used to predict the stability of a system.
… Zero Order Instruments: First Order Instruments:
It has ideal dynamic performance, because the output is proportional to the input for all frequencies and there is no amplitude or phase distortion.
Example: Linear Potentiometer
First Order Instruments:
It contains a single energy storage element.
Example: Low-pass RC filter.
… Second Order Instruments: Time Delay:
Instruments that requires second-order differential equation is required to describe its dynamic response.
Many medical instruments are second order or higher, and low pass.
Example: Force-measuring Spring Scale
Time Delay:
Instrument elements that give an output that is exactly the same as the input, except that it is delayed in time.
Example: Equipment that require significant signal processing schemes.
42 General Design Criteria and Process of Medical Instrument
Figure: Design process for medical instruments Choice and design of instruments are affected by signal factors, and also by environmental, medical, and economic factors.
43 Regulations of Medical Devices
The medical instrumentation industry in general and hospitals in particular are required to be most regulated industries.
This is because when instruments are made on human beings and by the human beings, the equipment should not only be safe to operate but must give intended performance so that the patients could be properly diagnosed and treated.
To minimize the problems various countries have introduced a large numbers of codes, standards and regulations for different types of equipment and facilities.
It is therefore, essential that engineers understand their significance and be aware of the issues that are brought about by technological and economical relaities.
44 Cont….
Regulations: A regulation is an organization’s way of specifying that some particular standard must be adhered to. These are rules normally promulgate by the government.
Codes: A systems of principles or regulations or a systematized body of law or an accumulation of a system of regulations and standards. In general, a code is compilation of standards relating to providing health care to the state population.
Specification: Documents used to control the procurement of equipment by laying down the performance and other associated criteria. These documents usually cover design criteria, system performance, materials and technical data.
Standards: A standard is a multi-party agreement for establishment of an arbitrary criterion for reference. Alternatively standard is prescribed set of rules, conditions or requirements concerned with the definition of terms, classification of components, delineation of procedures, specifications of materials, performance, design or operations, measurements of quality and quality in describing materials, products, systems, services or practice. Standards exist that address systems (protection of the electrical power distribution systems from faults), individuals (measure to reduce potential electric shock hazards) and protection of the environment (disposal of medical waste).
46 Types of Standards
There are in general three type of standards for medical devices:
Voluntary Standards: Developed through a consensus process where manufactures, users, consumers and government agencies participate.
Mandatory Standards: Required to be followed under law. They are incumbent on those to whom the standard is addressed and enforceable by the authority having jurisdiction
Proprietary Standards: Developed either by a manufacturer for its own internal use or by a trade association for use by its members.
47 Regulatory Requirements
In 1976 the United States Congress passed what are known as the Medical Device Amendments (Public Law ) to the Federal Food, Drug, and Cosmetics Act that dates back to the 1930s.
The primary purpose was to ensure the safety and efficacy of new medical devices prior to marketing of the device.
Medical devices were classified in two ways.
First, the division of such devices into Class I, II, and
III was based on the principle that devices that pose greater potential hazards should be subject to more regulatory requirements.
Second, seven categories were established: preamendment, postamendment, substantially equivalent, implant, custom, investigational, and transitional.
The seven categories into which medical devices are divided are described in Table, which also includes classification rules and examples.
Software used in medical devices has become an area of increasing concern.
Class I General Controls: Manufacturers are required to perform registration, premarketing notification, record keeping, labeling, reporting of adverse experiences, and good manufacturing practices. These controls apply to all three classes.
Class II Performance Standards: Apply to devices for reasonable assurance of safety and efficacy, and for which existing information is sufficient to establish a performance standard. However, until performance standards are developed by regulation, only general control apply.
Class III Premarketing Approval: Such approval is required for devices used in supporting or sustaining human life and preventing impairment of human health.
The FDA has extensively regulated these devices by requiring manufacturers to prove their safety and effectiveness prior to market release.
Lecture 5 Transcript
Lecture 5
Instrument performance is specified by range, resolution, accuracy, and precision.
Range is defined by the highest and lowest readings the instrument is expected to produce. The lowest reading, if zero, is often omitted: 0-20 psi or 20 psi. Other examples: 3000 microstrain, 10 degrees, 50 mm, 700 kPa.
Sensitivity is the smallest change that can be sensed by a sensor. Sensitivity typically decreases as range increases. Examples: 0.01 mm, 0.1 inch.
Resolution is the smallest change that can be displayed on a readout device. Resolution typically decreases as range increases. Examples: 0.01 mm, 0.1 Hz, 0.025% Full Scale.
Repeatability or Precision is the degree to which a reading deviates from the mean of a series of readings taken under identical conditions. This parameter is always expressed as a ± value, such as ± 0.5mm or ±0.25% FS.
Accuracy is the degree to which a reading deviates from an absolute value. Accuracy is always expressed as a ± value, such as ± 0.5mm or ±0.1 %FS (full scale).
Discussion
Costs generally increase with sensitivity, resolution, repeatability, and accuracy, so it is important to specify just the performance levels that are needed. Higher performance levels do not necessarily provide more useful information.
Sensitivity and resolution are similar because both refer to the smallest change that can be that can be sensed or displayed. Resolution is more common in specifications. A truly complete specification for resolution will include not only the resolution value but also the readout that was used: 1 arc second using EL/MEMS data recorder.
Repeatability and accuracy are similar parameters because both refer to deviation or error. In most geotechnical applications, it is sufficient to have instruments with good repeatability, since we are more concerned with changes than with absolute values. We compare current and intial readings to learn if pore-pressure has increased or if movement is occuring. The absolute value of the pore-pressure or the tilt of the inclinometer casing is of lesser interest.
Sensitivity and resolution are quite different from repeatability and accuracy. The first two are concerned with “smallest value” while the second two are concerned with “greatest error.” Sensitivity and resolution are usually many times smaller than repeatability and accuracy.
Static and Dynamic characteristics of Instruments
Characteristics of measurement systems
• To choose the one most suited to a particular measurement application, we have to know the system characteristics.
• The performance characteristics may be broadly divided into two groups, namely‘static’ and ‘dynamic’ characteristics
Static characteristics the performance criteria for the measurement of quantities that remain constant, or vary only quite slowly.
Dynamic characteristics the relationship between the system input and output when the measured quantity (measurand) is varying rapidly.
• In practice, the characteristics of the one group may well influence the characteristics of the other. In order to access overall instrument performance, however, the two groups of
characteristics are normally studied separately and then a semi-quantitative superposition is carried out.
1. Accuracy
• This is the closeness with which the measuring instrument can measure the ‘true value’ of the measurand under stated conditions of use, i.e. its ability to ‘tell the truth’.
• The accuracy of an instrument is quantified by the difference of its readings and the one given by the ultimate or primary standard.
Accuracy depends on inherent limitations of instrument and shortcomings in measurement
process.
Unit of accuracy:
1. Percentage of true value (% of T.V.) = (Measured value – True value) *100 True value
2. Percentage of Full Scale Deflection (% of fsd) = (Measured value – True value) *100
Maximum Scale value
2. Precision
• Precision is defined as the ability of instrument to reproduce a certain set of readings within given accuracy.
• Precision describes an instrument’s degree of random variations in its output when measuring a constant quantity.
• Precision depends upon repeatability.
3. Repeatability
• Repeatability is defined as ability of instrument to reproduce a group of measurements of same measured quantity, made by same observer, using same instrument, under same conditions.
Precision is often confused with accuracy. High precision does not imply anything about measurement accuracy.
Accuracy Precision
• Accuracy represents degree of correctness of the measured value w.r.t. true value.
• Accuracy of instrument depends on systematic errors.
• Precision represents degree of repeatability of several independent measurements
of desired input at the same reference conditions
• Precision of instruments depends on factors that cause random or accidental
errors.
Measuring a fixed target position Low precision, low accuracy
High precision, low accuracy
High precision,
High accuracy
4. Resolution (Discrimination)
• It is the minimum change or smallest increment in the measured value that can be detected with certainty by the instrument.
• It can be least count of instrument.
5. Dead Space : Threshold
Dead space/ Threshold is defined as the range of different input values over which there is no
change in output value.
6. Tolerance
– Tolerance is a term that is closely related to accuracy and defines the maximum error that
is to be expected in some value.
– Tolerance describes the maximum deviation of a manufactured component from some
specified value
7. Range or span
– The range or span of an instrument defines the minimum and maximum values of a quantity
that the instrument is designed to measure.
8. Linearity This is the closeness to a straight line of the relationship between the
true process variable and the measurement. i.e. deviation of transducer output curve from a specified straight line.
1. Independent of Input
2. Proportional to Input
3. Combined independent & proportional to Input.
Linearity is usually reported as non-linearity, which is the maximum of the deviation between the calibration curve and a straight line positioned so that the maximum deviation is minimized.
9. Sensitivity of measurement
The sensitivity of measurement is a measure of the change in instrument output that occurs when the quantity being measured changes by a given amount. Thus, sensitivity
is the ratio:
Static Sensitivity K = Change of Output Signal qo
Change in Input Signal qi
10. Reliability
Reliability is the probability that a device will adequately perform (as specified) for a period of time under specified operating conditions. Some sensors are required for safety or product quality, and therefore, they should be very reliable.
11. Instrument Drift
• It is defined as the variation of output for a given input caused due to change in sensitivity of the instrument due to certain interfering inputs like temperature changes, component
instabilities, etc.
• Prime sources occur as chemical structural changes and changing mechanical stresses.
• Drift is a complex phenomenon for which the observed effects are that the sensitivity and offset values vary.
• It also can alter the accuracy of the instrument differently at the various amplitudes of the signal present.
Effects of disturbance:
(a) zero drift; (b) sensitivity drift;
(c) zero drift plus sensitivity drift.
12. Hysteresis
• Careful observation of the output/input relationship of a block will sometimes reveal different results as the signals vary in direction of the movement.
• Mechanical systems will often show a small difference in length asthe direction of the applied force is reversed.
• The same effect arises as a magnetic field is reversed in a magnetic material.
• This characteristic is called hysteresis.
• Hysteresis is defined as the magnitude of error caused in the output for a given value of input, when this value is approached from opposite directions ; i.e. from ascending order & then descending order.
• Causes are backlash, elastic deformations, magnetic characteristics, frictional effects (mainly).
• Hysteresis can be eliminated by taking readings in both direction and then taking its arithmetic mean.
Instrument characteristic with hysteresis.
13. Backlash
• It is defined as the maximum distance or angle through which any part of mechanical system may be moved in one direction without causing motion of next part.
• Can be minimized if components are made to very close tolerances.
Errors are normally classified in three categories: systematic errors, random errors, and blunders.
Systematic Errors
Systematic errors are due to identified causes and can, in principle, be eliminated. Errors of this type result in measured values that are consistently too high or consistently too low. Systematic errors may be of four kinds:
1. Instrumental. For example, a poorly calibrated instrument such as a thermometer that reads 102 oC when immersed in boiling water and 2 oC when immersed in ice water at atmospheric pressure. Such a thermometer would result in measured values that are consistently too high.
2. Observational. For example, parallax in reading a meter scale.
3. Environmental. For example, an electrical power ìbrown outî that causes measured currents to be consistently too low.
4. Theoretical. Due to simplification of the model system or approximations in
the equations describing it. For example, if your theory says that the temperature of the surrounding will not affect the readings taken when it actually does, then this factor will introduce a source of error.
Random Errors
Random errors are positive and negative fluctuations that cause about one-half of the measurements to be too high and one-half to be too low. Sources of random errors cannot always be identified. Possible sources of random errors are as follows:
1. Observational. For example, errors in judgment of an observer when reading the scale of a measuring device to the smallest division.
2. Environmental. For example, unpredictable fluctuations in line voltage, temperature, or mechanical vibrations of equipment.
Random errors, unlike systematic errors, can often be quantified by statistical analysis, therefore, the effects of random errors on the quantity or physical law under investigation can often be determined.
Example to distinguish between systematic and random errors is suppose that you use a stop watch to measure the time required for ten oscillations of a pendulum. One source of error will be your reaction time in starting and stopping the watch. During one measurement you may start early and stop late; on the next you may reverse these errors. These are random errors if both situations are equally likely. Repeated
measurements produce a series of times
that are all slightly different. They vary in random vary about an average value.
If a systematic error is also included for example, your stop watch is not starting from zero, then your measurements will vary, not about the average value, but about a displaced value.
Blunders
A final source of error, called a blunder, is an outright mistake. A person may record a wrong value, misread a scale, forget a digit when reading a scale or recording a measurement, or make a similar blunder. These blunder should stick out like sore thumbs if we make multiple measurements or if one person checks the work of another. Blunders should not be included in the analysis of data.
Statistical analysis
Statistical analysis means investigating trends, patterns, and relationships using quantitative data. It is an important research tool used by scientists, governments, businesses, and other organizations.
To draw valid conclusions, statistical analysis requires careful planning from the very start of the research process. You need to specify your hypotheses and make decisions about your research design, sample size, and sampling procedure.
After collecting data from your sample, you can organize and summarize the data using descriptive statistics. Then, you can use inferential statistics to formally test hypotheses and make estimates about the population. Finally, you can interpret and generalize your findings.
This article is a practical introduction to statistical analysis for students and researchers. We’ll walk you through the steps using two research examples. The first investigates a potential cause-and-effect relationship, while the second investigates a potential correlation between variables.
In statistics reliability is the overall consistency of a measure. A measure is said to have a high reliability if it produces similar results under consistent conditions:
“It is the characteristic of a set of test scores that relates to the amount of random error from the measurement process that might be embedded in the scores. Scores that are highly reliable are precise, reproducible, and consistent from one testing occasion to another. That is, if the testing process were repeated with a group of test takers, essentially the same results would be obtained. Various kinds of reliability coefficients, with values ranging between 0.00 (much error) and 1.00 (no error), are usually used to indicate the amount of error in the scores.”
For example, measurements of people’s height and weight are often extremely reliable.
Types
There are several general classes of reliability estimates:
Inter-rater reliability assesses the degree of agreement between two or more raters in their appraisals. For example, a person gets a stomach ache and different doctors all give the same diagnosis.
Test-retest reliability assesses the degree to which test scores are consistent from one test administration to the next. Measurements are gathered from a single rater who uses the same methods or instruments and the same testing conditions. This includes intra-rater reliability.
Inter-method reliability assesses the degree to which test scores are consistent when there is a variation in the methods or instruments used. This allows inter-rater reliability to be ruled out. When dealing with forms, it may be termed parallel-forms reliability.
Internal consistency reliability, assesses the consistency of results across items within a test In statistics Accuracy
“Accuracy” refers to the provision of either measures of accuracy or precision (numerical results of the methods/processes for assessing the accuracy or precision of data) or qualitative assessment indicators. It may also be described in terms of the major sources of error that potentially cause inaccuracy. It includes providing the results of the assessment of source data for coverage, sampling error, response error and non-sampling error.
The accuracy of statistical information is the degree to which the information correctly describes the phenomena it was designed to measure. It is usually characterized in terms of error in statistical estimates and is traditionally decomposed into bias (systematic error) and variance (random error) components. It may also be described in terms of the major sources of error that potentially cause inaccuracy (e.g., coverage, sampling, non response, response)
Fidelity is the quality of faithfulness or loyalty. Its original meaning regarded duty in a broader sense than the related concept of fealty. Both derive from the Latin word fidēlis, meaning “faithful or loyal”. In the City of London financial markets it has traditionally been used in the sense encompassed in the motto “My word is my bond”.
Audio and electronics
Sound recording and reproduction
In audio, “fidelity” denotes how accurately a copy reproduces its source. In the 1950s, the terms “high fidelity” or “hi-fi” were popularized for equipment and recordings which exhibited more accurate sound reproduction. For example, a worn gramophone record will have a lower fidelity than one in good condition, and a recording made by a low budget record company in the early 20th century is likely to have significantly less audio fidelity than a good modern recording. Similarly in electronics, fidelity refers to the correspondence of the output signal to the input signal, rather than sound quality, as in the popular internet connection technology.
The term “lo-fi” has existed since at least the 1950s, shortly after the acceptance of “hi-fi”, but its definition evolved continuously between the 1970s and 2000s. In the 1976 edition of the Oxford Dictionary, lo-fi was added under the definition of “sound production less good in quality than ‘hi-fi,'” and in the glossary of the 1977 book The Tuning of the World, was defined as “unfavourable signal-to-noise ratio.” in 2003, the Oxford Dictionary added a second definition for the term—”a genre of rock music characterized by minimal production, giving a raw and unsophisticated sound”. A third was added in 2008: “unpolished, amateurish, or technologically unsophisticated, esp. as a deliberate aesthetic choice.
Speed of response
The time required for a system to react to some signal; for example, the delay time for a photon detector to react to a radiation pulse, or the time needed for a current or voltage in a circuit to reach a definite fraction of its final value as a result of an abrupt change in the electromotive force.
CLASSIFICATION OF THE LINEARIZATION
TECHNIQUES
Contrary to expectations, linearization techniques are not as novel as they seem to be. In fact, some of them were proposed before the transistor was used as an amplifier device, mainly in analog transmitters of the AM broadcasting.
In recent years, the increase of the high efficiency demands have result in specific efforts to best use the electromagnetic spectrum, involving high linear amplification and, consequently, entailing efficiency reductions. This has culminated in an ongoing research on linearization techniques focused on higher frequencies, bandwidths and efficiency rates.
The classification of linearization techniques, according to one of the most generalized tendency, can be divided into two groups.
In the first group an input signal is amplify while distortion components are generated. The aim of these techniques lies in canceling such distortion modifying the input signal or directly subtracting it from the output signal.
These linearization techniques are:
Feedback
Predistortion
Feedforward
The linearization techniques of the second group are commonly known as efficiency enhancement techniques. Load impedance modifications, supply source variations or output signal combinations are used in order to maximize the overall transmission efficiency or likewise, the linear performance.
Some of those techniques are:
Bypassing
Envelope Elimination and Restoration (EER)
Envelope tracking
Linear amplification using Nonlinear Components (LINC)
Doherty Method
Combined Analogue Locked Loop Universal Modulator (CALLUM)
Alternatively, the linearization can be differenced whether baseband or RF signals are used as input signal. In the first case, the linearization techniques can use any of the modulation techniques and make any frequency translations whereas in the second case they do not.
INTRODUCTION
DATA ACQUISITION is the process of sampling signals that measure real world physical conditions and converting the resulting samples into digital numeric values that can be manipulated by a computer.
Data acquisition systems (abbreviated with the acronym DAS or DAQ) typically convert analog waveforms into digital values for easy processing
The components of data acquisition systems include:
Sensors that convert physical parameters to electrical signals.
Signal conditioning circuitry to convert sensor signals into a form that can be converted to digital values.
Analog-to-digital converters, which convert conditioned sensor signals to digital values.
OBJECTIVE
DAS must acquire the necessary data, at correct speed and at correct time.
It must monitor the complete plant operation to maintain on line and safe operations.
It must be able to collect, summarise and store data for diagnosis of operation and record purpose.
It must be flexible and capable of being expanded for future requirements.
It must be able to compute unit performance indices using on-line, real time data.
It must be reliable, easy to operate and must be user friendly.
Lecture 6 Transcript
Lecture 6
Sensory System
The human body can achieve an understanding of the world through its sensory systems. Sensory systems are widespread throughout the body including those that detect the world directly from the outside (exteroreceptors), those that detect information from internal organs and processes (interoceptors), and those detecting sense of position and load (proprioception).
Sensory receptors occur in specialized organs such as the eyes, ears, nose, and mouth, as well as internal organs. Each receptor type conveys a distinct sensory modality to integrate into a single perceptual frame eventually. This information is achieved by the conversion of energy into an electrical signal by specialized mechanisms. In this report, we will discuss a basic overview of sensory systems, focusing on sensory receptors.
Classification of Receptors by Stimulus
Sensory receptors are primarily classified as chemoreceptors, thermoreceptors, mechanoreceptors, or photoreceptors.
Chemoreceptors detect the presence of chemicals.
Thermoreceptors detect changes in temperature.
Mechanoreceptors detect mechanical forces.
Photoreceptors detect light during vision.
More specific examples of sensory receptors are baroreceptors, propioceptors, hygroreceptors, and osmoreceptors.
Sensory receptors perform countless functions in our bodies mediating vision, hearing, taste, touch, and more.
Photoreceptor: A specialized neuron able to detect and react to light.
Mechanoreceptor: Any receptor that provides an organism with information about mechanical changes in its environment such as movement, tension, and pressure.
Baroreceptor: A nerve ending that is sensitive to changes in blood pressure.
Sensory receptors can be classified by the type of stimulus that generates a response in the receptor. Broadly, sensory receptors respond to one of four primary stimuli:
1. Chemicals (chemoreceptors)
2. Temperature (thermoreceptors)
3. Pressure (mechanoreceptors)
4. Light (photoreceptors)
A schematic of the classes of sensory receptors: Sensory receptor cells differ in terms of morphology, location, and stimulus.
All sensory receptors rely on one of these four capacities to detect changes in the environment, but may be tuned to detect specific characteristics of each to perform a specific sensory function. In some cases, the mechanism of action for a receptor is not clear. For example, hygroreceptors that respond to changes in humidity and osmoreceptors that respond to the osmolarity of fluids may do so via a mechanosensory mechanism or may detect a chemical characteristic of the environment.
Sensory receptors perform countless functions in our bodies. During vision, rod and cone photoreceptors respond to light intensity and color. During hearing, mechanoreceptors in hair cells of the inner ear detect vibrations conducted from the eardrum. During taste, sensory neurons in our taste buds detect chemical qualities of our foods including sweetness, bitterness, sourness, saltiness, and umami (savory taste). During smell, olfactory receptors recognize molecular features of wafting odors. During touch, mechanoreceptors in the skin and other tissues respond to variations in pressure.
Classification of Sensory Receptors
Adequate Stimulus
Adequate stimulus can be used to classify sensory receptors. A sensory receptor’s adequate stimulus is the stimulus modality for which it possesses the adequate sensory transduction apparatus.
Sensory receptors with corresponding stimuli to which they respond.
Receptor Stimulus
Apmullae of Lorenzini (primarily function as electroreceptors) Electric fields, salinity, and temperature
Baroreceptors Pressure in blood vessels
Chemo receptors Chemical stimuli
Electromagnetic radiation receptors Electromagnetic radiation
Electroreceptors Electrofields
Hydroreceptors Humidity
Infrared receptors Infrared radiation
Magnetoreceptors Magnetic fields
Mechanoreceptors Mechanical stress or strain
Nociceptors Damage or threat of damage to body tissues (leads to pain perception)
Osmoreceptors Osmolarity of fluids
Photoreceptors Visible light
Proprioceptors Sense of position
Thermoreceptors Temperature
Ultraviolet receptors Ultraviolet radiation
Location
Sensory receptors can be classified by location:
· Cutaneous receptors are sensory receptors found in the dermis or epidermis.
· Muscle spindles contain mechanoreceptors that detect stretch in muscles.
Morphology
Somatic sensory receptors near the surface of the skin can usually be divided into two groups based on morphology:
1. Free nerve endings characterize the nociceptors and thermoreceptors.
2. Encapsulated receptors consist of the remaining types of cutaneous receptors. Encapsulation exists for specialized functioning.
Rate of Adaptation
A tonic receptor is a sensory receptor that adapts slowly to a stimulus, while a phasic receptor is a sensory receptor that adapts rapidly to a stimulus.
Classification of Receptors by Location
Some sensory receptors can be classified by the physical location of the receptor.
Differentiate among sensory receptors by location
· Sensory receptors that share a common location often share a related function.
· Sensory receptors code four aspects of a stimulus: modality (or type), intensity, location, and duration.
· Cutaneous touch receptors and muscle spindle receptors are both mechanoreceptors, but they differ in location.
· cutaneous touch receptor: A type of sensory receptor found in the dermis or epidermis of the skin.
· muscle spindle: Sensory receptors within the belly of a muscle that primarily detect changes in the length of this muscle.
Lecture 7
Types of Receptors
As we exist in the world, our bodies are tasked with receiving, integrating, and interpreting environmental inputs that provide information about our internal and external environments. Our brains commonly receive sensory stimuli from our visual, auditory, olfactory, gustatory, and somatosensory systems.
Remarkably, specialized receptors have evolved to transmit sensory inputs from each of these sensory systems. Sensory receptors code four aspects of a stimulus:
1. Modality (or type)
2. Intensity
3. Location
4. Duration
Receptors are sensitive to discrete stimuli and are often classified by both the systemic function and the location of the receptor.
Sensory receptors are found throughout our bodies, and sensory receptors that share a common location often share a common function. For example, sensory receptors in the retina are almost entirely photoreceptors. Our skin includes touch and temperature receptors, and our inner ears contain sensory mechanoreceptors designed for detecting vibrations caused by sound or used to maintain balance.
Force -sensitive mechanoreceptors provide an example of how the placement of a sensory receptor plays a role in how our brains process sensory inputs. While the cutaneous touch receptors found in the dermis and epidermis of our skin and the muscle spindles that detect stretch in skeletal muscle are both mechanoreceptors, they serve discrete functions.
In both cases, the mechanoreceptors detect physical forces that result from the movement of the local tissue, cutaneous touch receptors provide information to our brain about the external environment, while muscle spindle receptors provide information about our internal environment.
Cellular
Lecture 7 Transcript
Lecture 7
The following is a detailed discussion of major sensory receptor types.
Receptors of vision
Retinal is the principal molecule of vision in the retina. It can absorb different frequencies of light. Its isomer (Cis-retinal) is present in rhodopsin, which is a photosensitive transmembrane G-protein that exists in rods and cones; it contains both cis-retinal and opsin.
Light is the stimulus and retinal is the receptor. The absorption of energy transforms cis-retinal into trans-retinal. With this conformational change, rhodopsin transforms into an activated form called meta-rhodopsin. Signal transduction then involves transducin, a multisubunit protein, by binding it to rhodopsin and causing conversion of GDP to GTP; this leads to the release of the alpha subunit allowing it to bind to cGMP phosphodiesterase – which lowers levels of cGMP. This signals closure of sodium channels that are otherwise open when it is dark. Interestingly, in this scenario, it is hyperpolarization that occurs with light signaling. This hyperpolarization results in a decreased amount of glutamate released to the postsynaptic membrane, signaling a change to the brain.
Receptors of hearing
To discuss how sound receptors work, first, we must mention the order of events. Sound waves travel to the ear creating a vibration in the tympanic membrane. This energy transforms into mechanical energy to the malleus, incus, and stapes. The stapes is in close proximity to the oval window, and it amplifies the mechanical energy to the cochlea, a fluid-filled structure with a fluid called perilymph, by directly pushing on it. The cochlea has three layers called scala vestibuli (the ascending portion), scala media, and scala tympani (the descending portion). The organ of Corti is on the basilar membrane surface, and it contains hair cells which are the primary receptors in sound signal creation. There are two varieties of hair cells: inner and outer. Inner cells transmit information to the auditory nerve, and outer cells mechanically amplify low-level sound entering the cochlea.
Inner hair cells have an attachment with a tectorial membrane to which they bend against with movement of the cochlear duct membranes and fluids. When the stereocilia on the hair cells bend towards the longest cilia, potassium and voltage-gated calcium channels open and ion influx increases resulting in depolarization. This depolarization allows for neurotransmitter release at the auditory nerve in the postsynapse, generating nerve impulses to be propagated from stereocilia of hair cells to the central nervous system via glutamate transmission. Discrimination of sound is via the location of the original nerve impulses from different areas of the cochlea.
Receptors of balance
The inner ear senses balance. With head motion or pressure impulses of sound, the endolymph vibrates and creates a stimulus for the receptors of the vestibular system – the utricle and saccule. Inside the utricle and saccule are maculae containing hair cells with a membranous covering of microscopic otoconia that detect motion of the endolymph. Those in the saccule help sense vertical accelerations whereas those in the utricle sense horizontal accelerations. With changes in position, and thus changes in fluid motion, the shifting of these hair cells causes opening of receptor channels leading to action potentials propagating from the hair cells to the auditory nerve. The rate of fluid motion, plus the quality of the fluid, gives us more information about the motion. While the utricle and saccule detect linear motion, the semicircular ducts detect rotations in a similar fashion.
Receptors of taste
Taste buds on the tongue and oropharynx help us enjoy and discriminate what we ingest.[6] The different tastes include sweet, salty, bitter, umami, and sour. A taste bud is a collection of taste cells that elongate at a tip to create a pore where stimuli may enter. Along these elongations are microvilli that protrude into the lumen of the mouth. On the other side of taste cells, there are nerve fibers that will eventually transmit the chemical gustatory message to the brain.
Just like most nervous tissue, with stimuli binding to the receptor, the receptor depolarizes and releases a neurotransmitter for a postsynaptic cell to uptake and transmit the message. Interestingly, higher concentrations create higher action potentials. The stimulus binding to each receptor varies for each taste. Sweet, umami, and bitter tastes are detected by G-protein coupled receptors (GPCRs). These receptors recognize and can discriminate a wide variety of substances by attaching to different domains on the receptor complex. Both saccharides, as well as proteins, trigger sweet sensations. Monosodium glutamate and aspartate in humans mostly trigger umami flavors. Because most bitter tastes are considered to be from toxic environmental compounds, these receptors can recognize a wide variety of stimuli; they include approximately 30 GPCR types. Sodium is the stimulus for salty taste, and protons are the stimulus for sour tastes. These stimuli cause ion channels to open, leading to depolarization and nerve signaling. Each taste bud has a variety of types of taste cells, and it depends on the concentration to determine which taste is perceived more strongly. When the receptor first encounters a signal, it displays a sharp increase in discharge, but then it steadily acclimates with continual exposure to the stimulus. Saliva, however, continually washes stimuli away from receptors. The terminal destination for these signals located is in the primary gustatory cortex in the frontal and insular lobes.
Receptors of smell
Smell occurs by binding of odorant molecules to receptors on the membrane of the cilia, causing an action potential that sends this information to the brain. These systems utilize G-protein receptors along with adenylate cyclase. Initially, scientists believed that molecules bound directly to receptors and that each receptor potentially identified a specific type of smell. However, Yoshioka et al. proposed a more plausible theory, because hydrogen and its isotope are sensed as entirely different smells. The authors relate this to a postulate called the “molecule vibration model.” When a substance is bound to its receptor, the substrate allows electrons to go down their gradient, and through their specific vibrational energies, it causes a flow of chemical changes and subsequent signaling to the brain.
Receptors on the skin
What follows is a discussion of the various receptors in the skin. Signals from the skin may be conveyed by physical change (mechanoreceptors), temperature (thermoreceptors), or pain (nociceptors). Sensory receptors exist in all layers of the skin.
Mechanoreceptors
There are six different types of mechanoreceptors detecting innocuous stimuli in the skin: those around hair follicles, Pacinian corpuscles, Meissner corpuscles, Merkel complexes, Ruffini corpuscles, and C-fiber LTM (low threshold mechanoreceptors). Mechanoreceptors respond to physical changes including touch, pressure, vibration, and stretch. Hair follicles can detect light touch; Meissner corpuscles in the dermal papillae detect indentation and slipping of objects; Pacinian corpuscles in the deeper dermis detect vibration; Merkel complexes in the basal epidermis create an understanding of structure and texture; Ruffini corpuscles detect stretch; C-fiber LTMs detect pleasant, light tactile sensations. Encapsulated receptors include Meissner corpuscle and the Pacinian corpuscle. In receptors that respond to stretch, there is a presence of “stretch-activated channels” that leads to depolarization via sodium influx.With smaller receptive fields, there is more precision in the detection of shape, form, and texture of stimuli.
Receptors that do not signal pain have lower thresholds of signaling activity. They use A fiber beta-type nerves and those with higher thresholds that signal pain use A-delta and C-fibers. The C and A-delta fibers respond to painful temperatures, mechanical forces, and chemicals.
Proprioceptors are also mechanoreceptors. Examples include muscle spindles and the Golgi tendon organ which respond to muscle contraction/relaxation and muscle strain respectively.
Thermoreceptors
The body has both warm and cold thermoreceptors. These receptors display a constant discharge to their specific temperatures, and when an experience of the opposite temperature occurs, there is a sudden ceasing of receptor discharge.
Cold receptors mainly sense temperatures between 25 to 30C. Temperatures below this cause release of bursting discharges. In touching dangerously hot objects (greater than 45C), there can be a brief sensation of cold due to the paradoxical firing of cold receptors. Warm receptors respond to the approximate temperature range of 30 to 46C. Higher temperatures may result in the decreased firing of these receptors.
Noxious heat is detectable by TRPV1, TRPM3 or ANO1 proteins, as well as capsaicin However, TRPV3 may be more responsible for detecting warm temperatures. There is redundancy in receptors; their exact mechanisms are unknown.
In contrast, for colder temperatures, it is believed that TRPM8 ion channels are one of many receptors responsible. These receptors are capable of detecting temperatures from below 16C to 26C. The belief is that other undiscovered receptors also have a role in cold detection.
Nociceptors
Nociceptors help signal pain that is related to temperature, pressure, and chemicals. As Dubin et al. discusses, most sensory receptors have low sensitivity to dictate all sensations to the brain. However, when it comes to pain, nociceptors only signal when the body has reached a point of tissue damage. Inflammatory markers increase during tissue damage, bind to receptors, and initiate pain signaling either externally or in the viscera. One of the ion channels families that are present on nociceptive neurons is called TRP (transient receptor potential) ion channels. Those signals that activate nociceptive receptors include extremes of temperatures, high pressures, and chemicals causing tissue damage . Different fibers relay pain information; these are A-delta and C fibers. These fibers differ in their myelination and nerve diameter and thus speed of transmission. Painful temperatures, uncomfortable pressures, and chemicals mostly use C-fibers. C-fibers vary to be able to sense all three types of stimuli. A-delta fibers are small and unmyelinated and are primarily involved in thermal and mechanosensitive pain. Nociceptors utilize mostly glutamate but also substance P, calcitonin gene-related peptide, and somatostatin to signal pain.
Additionally, the gate theory of pain proposes that innocuous stimuli may trump painful stimuli if both are present simultaneously.
Organ Systems Involved
Many sensations are generated and transmitted via specialized sensory organs, others, as viscera, contain nociceptors that activate following inflammation and tissue damage.
The sensory organ of the eye is the retina. In concert with the cornea and lens, light focuses on the vision board where information can transform from physical matter into electrical energy that lends itself to interpretation and understanding of the external world by the brain.
The skin possesses many sensory receptors in the epidermis, dermis, and hypodermis, which allows for discrimination of touch such as pressure differences (light vs. deep). Other qualities of the external world assessed by skin sensory receptors includes temperature, pain, and itch.
The inner ear houses hair cells in the cochlea to transduce sounds and the vestibule which mediates our sense of balance.
Smell is perceived through the binding of molecules to the chemoreceptors in the cilia of the olfactory epithelium in the nose.
The mediation of the sense of load and position is through the specialized structures of muscle spindles and joint capsules which contain mechanoreceptors that detect joint angle, muscle length, and force.
Taste appreciation occurs by dissolving of molecules in the taste buds in the mouth and oropharynx.
Function
These sensory systems are responsible for helping maintain homeostasis in the body and for allowing the body to best react to internal and external events.
Mechanism
All sensory signals begin as receptor potentials. These potentials lead to a release of a neurotransmitter that excites its corresponding nerve to send information to the brain. Just as with regular nerve signal transduction, creating a receptor potential requires surpassing a threshold level in the membrane potential. Interestingly, with sensory receptors, the more the threshold is exceeded, the higher the frequency of action potentials. All receptors share the property that they can detect signals that are weak and intense. However, there is a drop-off, or plateau when the stimulus has reached a level of maximum stimulation. At that point, the receptor is unable to increase its firing potential.
Sensory receptors display properties that are common to almost all receptor types, here we discuss some of them.
Receptive field
The site of a sensory neuron within its surrounding neuronal population is vital to determine the location of its neural message, whether tactile, visual, auditory, or others. The bodily area where a stimulus can affect a sensory receptor is called receptive field. This attribute in form of a physical dimension is vital to encode an accurate location of a stimulus. Areas that contain a higher number of small receptor fields can achieve better spatial resolution, evident in the fovea of the retina and portions of the skin such as fingertips and lips.
Labelled line principle
Sensory systems function by responding only to stimuli they are specific for and subsequently transducing it into a neural message which follows a discrete path to the brain. This constitutes the labelled line principle, which reserves the specificity of a receptor class in encoding a sensory modality to the designated brain area. This applies to somatosensory systems, as well as other specialized systems such as visual and auditory.
Adaptation is a common property of all sensory receptors. As a stimulus constantly excites the receptor, there will be a decrease in the rate of action potentials. Although receptors can adapt to a constant, unchanging stimulus, if there is a change, whether loss of the stimulus or change in intensity, the receptor is able to respond.
Topographical representation
Primary sensory cortical areas contain neurons that construct a location-specific or a quality-specific organization. Somatotopic representation displays in the primary sensory cortex by representing a distorted anatomical version of the body called sensory homunculus. Another example is the auditory system, where it displays a tonotopic map in the primary auditory cortex pertaining to sound frequencies.
Clinical Significance
Understanding the vast amount of sensory systems of the body is critical in the field of medicine. By discovering sensory receptors and investigating their mechanisms, we can understand the pathophysiology of various disorders that present. One of the highly-relevant topics is chronic pain syndrome, where the understanding nociceptors is vital in designing new pharmaceutical solutions and treatment plans for this debilitating problem.
Lecture 8 Transcript
Lecture 8
The Central Nervous System
The CNS consists of the brain and spinal cord, which are located in the dorsal body cavity. The brain is surrounded by the cranium, and the spinal cord is protected by the vertebrae. The brain is continuous with the spinal cord at the foramen magnum. In addition to bone, the CNS is surrounded by connective tissue membranes, called meninges, and by cerebrospinal fluid.
Meninges
Meninges of the CNS
There are three layers of meninges around the brain and spinal cord. The outer layer, the dura mater, is tough white fibrous connective tissue. The middle layer of meninges is arachnoid, which resembles a cobweb in appearance, is a thin layer with numerous threadlike strands that attach it to the innermost layer. The space under the arachnoid, the subarachnoid space, is filled with cerebrospinal fluid and contains blood vessels. The pia mater is the innermost layer of meninges. This thin, delicate membrane is tightly bound to the surface of the brain and spinal cord and cannot be dissected away without damaging the surface.
Meningiomas are tumors of the nerve tissue covering the brain and spinal cord. Although meningiomas are usually not likely to spread, physicians often treat them as though they were malignant to treat symptoms that may develop when a tumor applies pressure to the brain.
Brain
The brain is divided into the cerebrum, diencephalons, brain stem, and cerebellum.
Cerebrum
The largest and most obvious portion of the brain is the cerebrum, which is divided by a deep longitudinal fissure into two cerebral hemispheres. The two hemispheres are two separate entities but are connected by an arching band of white fibers, called the corpus callosum that provides a communication pathway between the two halves.
Each cerebral hemisphere is divided into five lobes, four of which have the same name as the bone over them: the fontal lobe, the parietal lobe, the occipital lobe, and the temporal lobe. A fifth lobe, the insula or Island of Reil, lies deep within the lateral sulcus.
Diencephalon
The diencephalons is centrally located and is nearly surrounded by the cerebral hemispheres. It includes the thalamus, hypothalamus, and epithalamus. The thalamus, about 80 percent of the diencephalons, consists of two oval masses of gray matter that serve as relay stations for sensory impulses, except for the sense of smell, going to the cerebral cortex. The hypothalamus is a small region below the thalamus, which plays a key role in maintaining homeostasis because it regulates many visceral activities. The epithalamus is the most dorsal portion of the diencephalons. This small gland is involved with the onset of puberty and rhythmic cycles in the body. It is like a biological clock.
Brain Stem
The brain stem is the region between the diencephalons and the spinal cord. It consists of three parts: midbrain, pons, and medulla oblongata. The midbrain is the most superior portion of the brain stem. The pons is the bulging middle portion of the brain stem. This region primarily consists of nerve fibers that form conduction tracts between the higher brain centers and spinal cord. The medulla oblongata, or simply medulla, extends inferiorly from the pons. It is continuous with the spinal cord at the foramen magnum. All the ascending (sensory) and descending (motor) nerve fibers connecting the brain and spinal cord pass through the medulla.
Cerebellum
The cerebellum, the second largest portion of the brain, is located below the occipital lobes of the cerebrum. Three paired bundles of myelinated nerve fibers, called cerebellar peduncles, form communication pathways between the cerebellum and other parts of the central nervous system.
Ventricles and Cerebrospinal Fluid
A series of interconnected, fluid-filled cavities are found within the brain. These cavities are the ventricles of the brain, and the fluid is cerebrospinal fluid (CSF).
Spinal Cord
The spinal cord extends from the foramen magnum at the base of the skull to the level of the first lumbar vertebra. The cord is continuous with the medulla oblongata at the foramen magnum. Like the brain, the spinal cord is surrounded by bone, meninges, and cerebrospinal fluid.
The spinal cord is divided into 31 segments with each segment giving rise to a pair of spinal nerves. At the distal end of the cord, many spinal nerves extend beyond the conus medullaris to form a collection that resembles a horse’s tail. This is the cauda equina. In cross section, the spinal cord appears oval in shape.
The spinal cord has two main functions:
Serving as a conduction pathway for impulses going to and from the brain. Sensory impulses travel to the brain on ascending tracts in the cord. Motor impulses travel on descending tracts.
Serving as a reflex center. The reflex arc is the functional unit of the nervous system. Reflexes are responses to stimuli that do not require conscious thought and consequently, they occur more quickly than reactions that require thought processes. For example, with the withdrawal reflex, the reflex action withdraws the affected part before you are aware of the pain. Many reflexes are mediated in the spinal cord without going to the higher brain centers.
The Peripheral Nervous System
The peripheral nervous system consists of the nerves that branch out from the brain and spinal cord. These nerves form the communication network between the CNS and the body parts. The peripheral nervous system is further subdivided into the somatic nervous system and the autonomic nervous system. The somatic nervous system consists of nerves that go to the skin and muscles and is involved in conscious activities. The autonomic nervous system consists of nerves that connect the CNS to the visceral organs such as the heart, stomach, and intestines. It mediates unconscious activities.
Structure of a Nerve
A nerve contains bundles of nerve fibers, either axons or dendrites, surrounded by connective tissue. Sensory nerves contain only afferent fibers, long dendrites of sensory neurons. Motor nerves have only efferent fibers, long axons of motor neurons. Mixed nerves contain both types of fibers.
A connective tissue sheath called the epineurium surrounds each nerve. Each bundle of nerve fibers is called a fasciculus and is surrounded by a layer of connective tissue called the perineurium. Within the fasciculus, each individual nerve fiber, with its myelin and neurilemma, is surrounded by connective tissue called the endoneurium. A nerve may also have blood vessels enclosed in its connective tissue wrappings.
Cranial Nerves
Twelve pairs of cranial nerves emerge from the inferior surface of the brain. All of these nerves, except the vagus nerve, pass through foramina of the skull to innervate structures in the head, neck, and facial region.
The cranial nerves are designated both by name and by Roman numerals, according to the order in which they appear on the inferior surface of the brain. Most of the nerves have both sensory and motor components. Three of the nerves are associated with the special senses of smell, vision, hearing, and equilibrium and have only sensory fibers. Five other nerves are primarily motor in function but do have some sensory fibers for proprioception. The remaining four nerves consist of significant amounts of both sensory and motor fibers.
Acoustic neuromas are benign fibrous growths that arise from the balance nerve, also called the eighth cranial nerve or vestibulocochlear nerve. These tumors are non-malignant, meaning that they do not spread or metastasize to other parts of the body. The location of these tumors is deep inside the skull, adjacent to vital brain centers in the brain stem. As the tumors enlarge, they involve surrounding structures which have to do with vital functions. In the majority of cases, these tumors grow slowly over a period of years. In other cases, the growth rate is more rapid and patients develop symptoms at a faster pace. Usually, the symptoms are mild and many patients are not diagnosed until some time after their tumor has developed. Many patients also exhibit no tumor growth over a number of years when followed by yearly MRI scans.
Spinal Nerves
Thirty-one pairs of spinal nerves emerge laterally from the spinal cord. Each pair of nerves corresponds to a segment of the cord and they are named accordingly. This means there are 8 cervical nerves, 12 thoracic nerves, 5 lumbar nerves, 5 sacral nerves, and 1 coccygeal nerve.
Each spinal nerve is connected to the spinal cord by a dorsal root and a ventral root. The cell bodies of the sensory neurons are in the dorsal root ganglion, but the motor neuron cell bodies are in the gray matter. The two roots join to form the spinal nerve just before the nerve leaves the vertebral column. Because all spinal nerves have both sensory and motor components, they are all mixed nerves.
Autonomic Nervous System
The autonomic nervous system is a visceral efferent system, which means it sends motor impulses to the visceral organs. It functions automatically and continuously, without conscious effort, to innervate smooth muscle, cardiac muscle, and glands. It is concerned with heart rate, breathing rate, blood pressure, body temperature, and other visceral activities that work together to maintain homeostasis.
The autonomic nervous system has two parts, the sympathetic division and the parasympathetic division. Many visceral organs are supplied with fibers from both divisions. In this case, one stimulates and the other inhibits. This antagonistic functional relationship serves as a balance to help maintain homeostasis.
Lecture 9 Transcript
Lecture 9
Neural Control Mechanisms
Neurons generate electric signals that pass from one end of the neuron to another
Structure
A neuron has: (1) a cell body containing the cell organelles, (2) dendrites, branched outgrowths from the cell body that receive inputs over its vast surface area, (3) an axon, a single long process that extends from the cell body to its target cells, (4) an axon terminal which releases neurotransmitters that diffuse through extracellular space to trigger cells opposite the terminal.
A nerve fiber is a single axon while a nerve is a bundle of axons bound together by connective tissue.
Axons of some neurons are covered by myelin, a layer of plasma membranes with supporting cells that are called glial cells in CNS and Schwann cells in the peripheral nervous system. The spaces between adjacent sections of myelin where the axon is exposed to extracellular fluid are called nodes of Ranvier. Myelin speeds up the conduction of electric signals.
Glial Cells
Glial cells physically and metabolically support neurons. Oligodendroglia form the myelin covering of CNS axons. Astroglia regulates the composition of extracellular fluid in CNS. Microglia perform immune functions.
Functional Classes of Neurons
3 types:
Afferent neurons that have sensory receptors at their ends and convey signals from tissues and organs into CNS
Efferent neurons that transmit signals from CNS to effector cells
Interneurons that connect neurons within CNS.
The junction between two neurons, where one neuron alters the activity of another (via a neurotransmitter) is called a synapse. A neuron conducting signals toward a synapse is called a presynaptic neuron while a neuron conducting signals away from a synapse is a postsynaptic neuron.
Neural Growth and Regeneration
The development of neurons is guided by neurotropic (neurogrowth) factors. Neurons outside the CNS can repair themselves but neurons within the CNS cannot.
Membrane Potentials
The difference in the amount of charge between two points is called a potential difference and its unit of measurement is volt. This difference tends to make the charge low, producing an electric current. The material through which it is flowing obstructs the current and this is called resistance. Ohm’s law gives the relationship
I = E/R
where:
I = electric current
E = electric potential
R = resistance
Materials with high resistance are called insulators, and those with low resistance are called conductors. Water with dissolved ions (electrolytes) is a good conductor while lipids are insulators. Intra- and extracellular fluids have numerous ions and are therefore conductors while the plasma membrane separating them is an insulator.
Resting membrane potential
The potential difference across the plasma membrane of a cell under resting conditions inside of the cell is negatively charged with respect to outside. The magnitude of the potential is determined by (1) differences in specific ion concentrations in intra- and extracellular fluids, and (2) differences in membrane permeabilities to different ions as a function of the number of open ion channels for these ions. Na+ and K+ play the most important roles in generating the resting membrane potential. Nat is greater outside while K+ is greater inside the cell. K+ moves out of the cell and Na+ moves into the cell down their concentration gradients but an intracellular concentration of these two ions is kept constant by an active transport system that pumps Na+ out of the cell and K+ into it. However, the pump brings out 3 Na+ for every 2 K+ it pumps in, making inside of the cell negative.
Graded and action potentials
Graded potentials are changes in membrane potential confined to a small region of the plasma membrane. The magnitude of these potentials is related to the magnitude of the initiating stimulus. They initiate a signal. Action potentials are large, rapid alterations in the membrane potential. Membranes capable of producing action potentials are called excitable membranes. Examples are membranes in nerve and muscle cells.
Ionic basis of action potential
During an action potential, voltage-gated Na+ channels open and allow a large influx of Na+ ions into the cell, making inside of the cell less negative and this is called depolarization. The membrane starts returning rapidly to the resting membrane potential because Na+ channels close, voltage-gated K+ channels open, K+ moves out and this is called repolarization. However, so much K+ moves out that inside of the cell becomes more negative than the original resting membrane potential and this is called hyperpolarization. In some cells, Ca2+ channels serve the same function as Na+ channels. Local anesthetics block the Na+ channels and prevent an action potential.
Threshold and all-or-none response
The potential at which a membrane is depolarized to generate an action potential is called the threshold potential and stimulus that is strong enough to depolarize the membrane is called a threshold stimulus.
A stimulus of more than threshold magnitude also elicits an action potential of the same amplitude as that caused by a threshold stimulus. This is because once the threshold is reached membrane events are no longer dependent upon the stimulus strength. Therefore, action potentials occur maximally or do not occur at all and this is called an all-or-none response. This is why a single action potential cannot convey information about the magnitude of the stimulus that initiated it
Refractory periods
The period after an action potential when a second stimulus will, not produce a second action potential is called an absolute refractory period. It occurs because once the voltage-gated Na+ channels close, the membrane needs to repolarize before the channels can open once again. Following the absolute refractory period, there is an interval during which a second action potential can be produced only is the stimulus strength is greater than usual. This is called relative refractory period and is a result of hyperpolarization.
Initiation of action potential
The initial depolarization in afferent neurons is achieved by either a graded potential called receptor potential in the receptors or by a spontaneous change in the neuron membrane potential called pacemaker potential.
Action potential propagation
Since a neuron is a long cell, it gets depolarized part by part and not all at once. The area of the membrane that gets depolarized has a difference in potential with the adjacent area of the membrane that is still at resting potential causing a local current. This current then depolarizes the adjacent resting membrane and a new action potential is generated there and so on. Because depolarization of an area is followed by a refractory period, the action potential moves unidirectionally. The velocity of action potential propagation is positively correlated with fiber diameter because a larger fiber offers less resistance. Myelin sheath, being an insulator prevents the flow of ions between intra- and extracellular compartments. Therefore, action potentials occur only at the non-insulated nodes of Ranvier and this jump of action potentials from one node to another is called saltatory conduction. By preventing leakage of charge, myelin increases the speed of propagation, enabling axons to be thinner.
Synapses
A synapse is a junction between two neurons, where the electrical activity in the presynaptic neuron influences the electrical activity in the postsynaptic neuron. The influence can be either excitatory or inhibitory. If many presynaptic cells affect a single postsynaptic cell it is called convergence and allows information from many sources to influence the activity of one cell. If a single presynaptic cell affects many postsynaptic cells it is called divergence and allows one information source to affect multiple pathways.
Functional anatomy of synapses
At electric synapses, the pre- and postsynaptic cells are joined by gap junctions, allowing action potentials to flow directly across the junction. Such synapses are rare.
At chemical synapses, the axon of the presynaptic neuron ends in a swelling called the axon terminal and an extracellular space called the synaptic cleft separates the pre- and postsynaptic neurons, preventing direct propagation of current between them. Signals are transmitted across the synaptic cleft by a chemical messenger – a neurotransmitter – released from the presynaptic axon terminal and bound by receptors at the postsynaptic cell. Most chemical synapses operate in only direction.
Neurotransmitters in axon terminals are stored in membrane-bound synaptic vesicles that are docked at the synaptic membrane. When an action potential depolarizes the axon terminal, voltage-gated Ca2+ channels in the membrane open, and Ca2+ diffuses from extracellular space into the axon terminal. The Ca2+ induce reactions that allow the vesicles to fuse with the plasma membrane and liberate their contents into the synaptic cleft by exocytosis.
Excitatory chemical synapses
The activated receptor on the postsynaptic membrane opens Na+ channels. There is a net movement of Na+ ions into the cell, resulting in depolarization. This potential change in the postsynaptic neuron is called an excitatory postsynaptic potential (EPSP). It is a graded potential.
Inhibitory chemical synapses
The activated receptor on the postsynaptic membrane opens Cl- channels. There is a net movement of Cl- ions into the cell, resulting in hyperpolarization. The potential change in the postsynaptic neuron is called an inhibitory postsynaptic potential (IPSP). It is a graded potential.
Activation of the postsynaptic cell
In most neurons, one EPSP is not enough to cross the threshold in the postsynaptic neuron and only the combined effects of many excitatory synapses can initiate an action potential. If a number of EPSPs arriving at different times create a depolarization it is called a temporal summation. If a number of EPSPs arriving at different locations create a depolarization, it is called a spatial summation. IPSPs also show similar summations but the effect is a hyperpolarization.
Neurotransmitters and Neuromodulators
Neuromodulators modify the postsynaptic cell’s response to neurotransmitters or change the presynaptic cell’s synthesis, release or metabolism of the neurotransmitter.
Acetylcholine (Ach)
Major neurotransmitter. Fibers that release ACh are called cholinergic fibers. Acetylcholine is degraded by the enzyme, acetylcholinesterase.
Biogenic amines
Biogenic amines are neurotransmitters containing an amino group. Catecholamines such as dopamine, norepinephrine and epinephrine, serotonin. Nerve fibers that release epinephrine and norepinephrine are called adrenergic and noradrenergic fibers respectively.
Amino acid neurotransmitters
Amino acid neurotransmitters are the most prevalent neurotransmitters in CNS. Glutamate, aspartate GABA (gamma-aminobutyric acid), glycine,
Neuropeptides
Neuropeptides are composed of two or more amino acids. Neurons releasing neuropeptides are called peptidergic. Beta-endorphin, dynorphin, enkephalins.
Nitric oxide, ATP, adenine also act as neurotransmitters.
Neuroeffector communication
Many neurons of the peripheral nervous system end at neuroeffector junctions on muscle and gland cells. Neurotransmitters released by these efferent neurons then activate the target cell.
Structure of the Nervous System
A group of nerve fibers traveling together in the CNS is called a pathway or tract and if it joins the left and the right halves, it is called a commissure.
Information in CNS passes along two types of pathways:
Long neural pathways in which neurons with long axons carry information directly between the brain and spinal cord or between different regions of the brain. There is no alteration in the transmitted information.
Multineuronal or multisynaptic pathway. Made up of many neurons or synapses. New information can be integrated into the transmitted information.
Cell bodies of neurons having similar function cluster together and such clusters are called ganglia in the peripheral nervous system and nuclei in the CNS.
CNS: spinal cord
The spinal cord lies within the vertebral column. The central gray matter is composed of interneurons, cell bodies, dendrites, and glial cells. This is surrounded by white matter composed of myelinated axons of interneurons. The fiber tracts either descend to relay information from the brain or ascend to relay information to the brain or transmit information across different levels of the spinal cord.
Afferent fibers enter from the peripheral system enter on the dorsal side of the cord via dorsal roots and form the dorsal root ganglia. Efferent fibers leave the cord on the ventral side via ventral roots. Dorsal and ventral roots from the same level combine to form a spinal nerve outside the cord, one on each side. 31 pairs of spinal nerves are designated by 4 levels of exit – cervical (8), thoracic (12), lumbar (5), and sacral (5).
CNS: brain
Brainstem: Consists of midbrain, pons and medulla oblongata. It contains the reticular formation, a bundle of axons that is involved in motor functions, cardiovascular and respiratory control, etc.
Cerebellum: An important center for coordinating movements and for controlling balance and posture.
Forebrain: The larger component of the forebrain, the cerebrum consists of the right and left cerebral hemispheres that have an outer shell of gray matter the cerebral cortex. Each hemisphere is divided into 4 lobes: frontal, parietal, occipital and temporal. The cortex is the most complex integrating area. The central core of the brain is formed by the diencephalon consisting of the thalamus – a collection of several large nuclei, and the hypothalamus – the master command center for neural and endocrine coordination.
Peripheral nervous system
Transmits signals between the CNS and receptors/effectors. Consists of 12paairs of cranial nerves that connect with the brain and 31 pairs of spinal nerves that connect with the spinal cord.
The efferent system is further divided into a somatic and an autonomic system.
Somatic nervous system
Innervates skeletal muscles. Consists of myelinated axons without any synapses. The activity of these neurons leads to excitation (contraction) of skeletal muscles and therefore they are called motor neurons. They are never inhibitory.
Autonomic nervous system
Innervates smooth and cardiac muscles. Parallel chains, each with two neurons, connect the CNS and effector cells. The synapse between these two neurons is called the autonomic ganglion, the nerve fibers between the CNS and the ganglion are called pre-ganglionic fibers and those between the ganglion and the effector cells are called post-ganglionic fibers.
Further divided into sympathetic (fight or flight) and parasympathetic (rest and relax) components.
Sympathetic ganglia lie close to the spinal cord while parasympathetic ganglia lie close to the organs. The sympathetic system is arranged to act as a single unit while the parasympathetic system is arranged such that the parts can act independently. The sympathetic system is involved in responses to stress. Many organs and glands receive a dual innervation from both sympathetic and parasympathetic fibers. The two systems generally have opposite effects and work together to regulate a response. Most autonomic responses usually occur without conscious control.
Blood supply, blood-brain barrier and cerebrospinal fluid
The neural tissue of the CNS is covered by 3 membranes called meninges – the outermost dura mater, the middle arachnoid, and the inner pia mater. The space between the pia and the arachnoid, the subarachnoid space, is filled with cerebrospinal fluid (CSF). It acts as a shock absorber for neural tissue.
The brain is highly dependent on a continuous supply of glucose and oxygen via blood. It has little stored glycogen.
The exchange of substances between the blood and extracellular fluid in CNS is highly restricted via a complex group of blood-brain barrier mechanisms. The CSF and the extracellular fluid in the brain are in diffusion equilibrium with each other but maintain a difference with the blood.
Lecture 10 Transcript
Lecture No.-10
Lecture 10
Chemoreceptors
One way in which breathing is controlled is through feedback by chemoreceptors. There are two kinds of respiratory chemoreceptors: arterial chemoreceptors, which monitor and respond to changes in the partial pressure of oxygen and carbon dioxide in the arterial blood, and central chemoreceptors in the brain, which respond to changes in the partial pressure of carbon dioxide in their immediate environment. Ventilation levels behave as if they were regulated to maintain a constant level of carbon dioxide partial pressure and to ensure adequate oxygen levels in the arterial blood. Increased activity of chemoreceptors caused by hypoxia or an increase in the partial pressure of carbon dioxide augments both the rate and depth of breathing, which restores partial pressures of oxygen and carbon dioxide to their usual levels. On the other hand, too much ventilation depresses the partial pressure of carbon dioxide, which leads to a reduction in chemoreceptor activity and a diminution of ventilation. During sleep and anesthesia, lowering carbon dioxide levels three to four millimetres of mercury below values occurring during wakefulness can cause a total cessation of breathing (apnea).
Peripheral chemoreceptors
Hypoxia, or the reduction of oxygen supply to tissues to below physiological levels (produced, for example, by a trip to high altitudes), stimulates the carotid and aortic bodies, the principal arterial chemoreceptors. The two carotid bodies are small organs located in the neck at the bifurcation of each of the two common carotid arteries into the internal and external carotid arteries. This organ is extraordinarily well perfused and responds to changes in the partial pressure of oxygen in the arterial blood flowing through it rather than to the oxygen content of that blood (the amount of oxygen chemically combined with hemoglobin). The sensory nerve from the carotid body increases its firing rate hyperbolically as the partial pressure of oxygen falls. In addition to responding to hypoxia, the carotid body increases its activity linearly as the partial pressure of carbon dioxide in arterial blood is raised. This arterial blood parameter rises and falls as air enters and leaves the lungs, and the carotid body senses these fluctuations, responding more to rapid than to slow changes in the partial pressure of carbon dioxide. Larger oscillations in the partial pressure of carbon dioxide occur with breathing as metabolic rate is increased. The amplitude of these fluctuations, as reflected in the size of carotid body signals, may be used by the brain to detect changes in the metabolic rate and to produce appropriate adjustment in ventilation.
The carotid body communicates with medullary respiratory neurons through sensory fibres that travel with the carotid sinus nerve, a branch of the glossopharyngeal nerve. Microscopically, the carotid body consists of two different types of cells. The type I cells are arranged in groups and are surrounded by type II cells. The type II cells are generally not thought to have a direct role in chemoreception. Fine sensory nerve fibres are found in juxtaposition to type I cells, which, unlike type II cells, contain electron-dense vesicles. Acetylcholine, catecholamines, and neuropeptides such as enkephalins, vasoactive intestinal polypeptide, and substance P, are located within the vesicles. It is thought that hypoxia and hypercapnia (excessive carbon dioxide in the blood) cause the release of one or more of these neuroactive substances from the type I cells, which then act on the sensory nerve. It is possible to interfere independently with the responses of the carotid body to carbon dioxide and oxygen, which suggests that the same mechanisms are not used to sense or transmit changes in oxygen or carbon dioxide. The aortic bodies located near the arch of the aorta also respond to acute changes in the partial pressure of oxygen, but less well than the carotid body responds to changes in the partial pressure of carbon dioxide. The aortic bodies are responsible for many of the cardiovascular effects of hypoxia.
Central chemoreceptors
Carbon dioxide is one of the most powerful stimulants of breathing. As the partial pressure of carbon dioxide in arterial blood rises, ventilation increases nearly linearly. Ventilation normally increases by two to four litres per minute with each one millimetre of mercury increase in the partial pressure of carbon dioxide. Carbon dioxide increases the acidity of the fluid surrounding the cells but also easily passes into cells and thus can make the interior of cells more acid. It is not clear whether the receptors respond to the intracellular or extracellular effects of carbon dioxide or acidity.
Even if both the carotid and aortic bodies are removed, inhaling gases that contain carbon dioxide stimulates breathing. This observation shows that there must be additional receptors that respond to changes in the partial pressure of carbon dioxide. Current thinking places these receptors near the undersurface (ventral part) of the medulla. However, microscopic examination has not conclusively identified specific chemoreceptor cells in this region. The same areas of the ventral medulla also contain vasomotor neurons that are concerned with the regulation of blood pressure. Some investigators suspect that respiratory responses produced at the ventral medullary surface are direct and are caused by interference with excitatory and inhibitory inputs to respiration from these vasomotor neurons. They further suspect that respiratory chemoreceptors that respond to carbon dioxide are more diffusely distributed in the brain.
thermoreceptor is a non-specialised sense receptor, or more accurately the receptive portion of a sensory neuron, that codes absolute and relative changes in temperature, primarily within the innocuous range. In the mammalian peripheral nervous system, warmth receptors are thought to be unmyelinated C-fibres (low conduction velocity), while those responding to cold have both C-fibers and thinly myelinated A delta fibers (faster conduction velocity).The adequate stimulus for a warm receptor is warming, which results in an increase in their action potential discharge rate. Cooling results in a decrease in warm receptor discharge rate. For cold receptors their firing rate increases during cooling and decreases during warming. Some cold receptors also respond with a brief action potential discharge to high temperatures, i.e. typically above 45 °C, and this is known as a paradoxical response to heat. The mechanism responsible for this behavior has not been determined.
Location
In humans, temperature sensation enters the spinal cord along the axons of Lissauer’s tract that synapse on first order neurons in grey matter of the dorsal horn, one or two vertebral levels up. The axons of these second order neurons then decussate, joining the spinothalamic tract as they ascend to neurons in the ventral posterolateral nucleus of the thalamus.
In mammals, temperature receptors innervate various tissues including the skin (as cutaneous receptors), cornea and urinary bladder. Neurons from the pre-optic and hypothalamic regions of the brain that respond to small changes in temperature have also been described, providing information on core temperature. The hypothalamus is involved in thermoregulation, the thermoreceptors allowing feed-forward responses to a predicted change in core body temperature in response to changing environmental conditions.
Structure
Thermoreceptors have been classically described as having ‘free’ non-specialized endings; the mechanism of activation in response to temperature changes is not completely understood.
Thermoreception
Cold-sensitive thermoreceptors give rise to the sensations of cooling, cold and freshness. In the cornea cold receptors are thought to respond with an increase in firing rate to cooling produced by evaporation of lacrimal fluid ‘tears’ and thereby to elicit a blink reflex. Other thermoreceptors will react to opposite triggers and give rise to heat and in some cases even burning sensations. This is often experienced when coming in contact with capsaicin, an active chemical commonly found in red chili peppers. When coming in contact with your tongue (or any internal surface), the capsaicin de-polarizes the nerve fibers, allowing sodium and calcium into the fibers. In order for fibers to do so, they must have a specific thermoreceptor. The thermoreceptor reacting to capsaicin and other heat producing chemicals is known as TRPV1. In response to heat, the TRPV1 receptor opens up passages that allow ions to pass through, causing the sensation of heat or burning. TRPV1 also has a molecular cousin, TRPM8. Unlike TRPV1, TRPM8 produces cooling sensations as mentioned previously. Similar to TRPV1, TRPM8 responds to a certain chemical trigger by opening its ion pathways. In this case, the chemical trigger is often menthol or other cooling agents. Studies performed on mice determined that the presence of both these receptors allows for a gradient of temperature sensing. Mice lacking the TRPV1 receptor were still capable of determining areas significantly colder than on a heated platform. Mice lacking the TRPM8 receptor however, were not able to determine the difference between a warm platform and a cold platform, suggesting we rely on TRPM8 to determine cold feelings and sensations.[2][3]
Distribution
Warm and cold receptors play a part in sensing innocuous environmental temperature. Temperatures likely to damage an organism are sensed by sub-categories of nociceptors that may respond to noxious cold, noxious heat or more than one noxious stimulus modality (i.e., they are polymodal). The nerve endings of sensory neurons that respond preferentially to cooling are found in moderate density in the skin but also occur in relatively high spatial density in the cornea, tongue, bladder, and facial skin. The speculation is that lingual cold receptors deliver information that modulates the sense of taste; i.e. some foods taste good when cold, while others do not.
Mechanism of transduction
This area of research has recently received considerable attention with the identification and cloning of the Transient Receptor Potential (TRP) family of proteins. The transduction of temperature in cold receptors is mediated in part by the TRPM8 channel. This channel passes a mixed inward cationic (predominantly carried by Na+ ions although the channel is also permeable to Ca2+) current of a magnitude that is inversely proportional to temperature. The channel is sensitive over a temperature range spanning about 10-35 °C. TRPM8 can also be activated by the binding of an extracellular ligand. Menthol can activate the TRPM8 channel in this way. Since the TRPM8 is expressed in neurons whose physiological role is to signal cooling, menthol applied to various bodily surfaces evokes a sensation of cooling. The feeling of freshness associated with the activation of cold receptors by menthol, particularly those in facial areas with axons in the trigeminal (V) nerve, accounts for its use in numerous toiletries including toothpaste, shaving lotions, facial creams and the like.
Another molecular component of cold transduction is the temperature dependence of so-called leak channels which pass an outward current carried by potassium ions. Some leak channels derive from the family of two-pore (2P) domain potassium channels. Amongst the various members of the 2P-domain channels, some close quite promptly at temperatures less than about 28 °C (e.g. TRAAK, TREK). Temperature also modulates the activity of the Na+/K+-ATPase. The Na+/K+-ATPase is a P-type pump that extrudes 3Na+ ions in exchange for 2K+ ions for each hydrolytic cleavage of ATP. This results in a net movement of positive charge out of the cell, i.e. a hyperpolarizing current. The magnitude of this current is proportional to the rate of pump activity.
It has been suggested that it is the constellation of various thermally sensitive proteins together in a neuron that gives rise to a cold receptor.[4] This emergent property of the neuron is thought to comprise, the expression of the aforementioned proteins as well as various voltage-sensitive channels including the hyperpolarization-activated, cyclic nucleotide-gated (HCN) channel and the rapidly activating and inactivating transient potassium channel
Lecture 11 Transcript
Ion-exchange membrane
An ion-exchange membrane is a semi-permeable membrane that transports certain dissolved ions, while blocking other ions or neutral molecules.
Ion-exchange membranes are therefore electrically conductive. They are often used in desalination and chemical recovery applications, moving ions from one solution to another with little passage of water.
Important examples of ion-exchange membranes include the proton-exchange membranes, that transport H+ cations, and the anion exchange membranes used in certain alkaline fuel cells to transport OH−anions.
Structure and composition
An ion-exchange membrane is generally made of organic or inorganic polymer with charged (ionic) side groups, such as ion-exchange resins. Anion-exchange membranes contain fixed cationic groups with predominantly mobile anions; because anions are the majority species, most of the conductivity is due to anion transport. The reverse holds for cation-exchange membranes.
The so-called heterogeneous ion-exchange membranes have low cost and a thicker composition with higher resistance and a rough surface that can be subject to fouling. Homogeneous membranes are more expensive, but have a thinner composition with lower resistance and a smooth surface, less susceptible to fouling. Homogeneous membrane surfaces can be modified to alter the membrane permselectivity to protons, monovalent ions, and divalent ions.
Selectivity
The selectivity of an ion-exchange membrane is due to Donnan equilibrium and not due to physically blocking or electrostatically excluding specific charged species.
The selectivity to the transport of ions of opposite charges is called its permselectivity.
Applications
Ion-exchange membranes are traditionally used in electrodialysis or diffusion dialysis by means of an electrical potential or concentration gradient, respectively, to selectively transport cationic and anionic species. When applied in an electrodialysis desalination process, anion- and cation-exchange membranes are typically arranged in an alternating pattern between two electrodes (an anode and a cathode) within the electrodialysis stack. A galvanic potential is supplied as a voltage generated at the electrodes.
A typical industrial electrodialysis stack consists of two chambers: a product-water chamber and a concentrate-reject chamber. During stack operation, salts are transferred from the product to the concentrate. As a result, the reject stream is concentrated up while the product stream is desalted.
Exemplary applications of ion-exchange membranes utilized in electrodialysis and EDR include seawater desalination, industrial wastewater treatment of highly scaling waters, food and beverage production, and other industrial wastewaters.
Enzymes
Enzymes are proteins that help speed up chemical reactions in our bodies. Enzymes are essential for digestion, liver function and much more. Too much or too little of a certain enzyme can cause health problems. Enzymes in our blood can also help healthcare providers check for injuries and diseases.
APPOINTMENTS & ACCESS
CONTACT US
What are enzymes?
Enzymes are proteins that help speed up metabolism, or the chemical reactions in our bodies. They build some substances and break others down. All living things have enzymes.
Our bodies naturally produce enzymes. But enzymes are also in manufactured products and food.
What do enzymes do?
One of the most important roles of enzymes is to aid in digestion. Digestion is the process of turning the food we eat into energy. For example, there are enzymes in our saliva, pancreas, intestines and stomach. They break down fats, proteins and carbohydrates. Enzymes use these nutrients for growth and cell repair.
Enzymes also help with:
Breathing.
Building muscle.
Nerve function.
Ridding our bodies of toxins.
What are the different types of enzymes?
There are thousands of individual enzymes in the body. Each type of enzyme only has one job. For example, the enzyme sucrase breaks down a sugar called sucrose. Lactase breaks down lactose, a kind of sugar found in milk products.
Some of the most common digestive enzymes are:
Carbohydrase breaks down carbohydrates into sugars.
Lipase breaks down fats into fatty acids.
Protease breaks down protein into amino acids.
PARTS OF ENZYMES
What are the parts of an enzyme?
Each enzyme has an “active site.” This area has a unique shape. The substance an enzyme works on is a substrate. The substrate also has a unique shape. The enzyme and the substrate must fit together to work.
How do temperature and pH affect enzymes?
Enzymes need the right conditions to work. If conditions aren’t right, enzymes can change shape. Then, they no longer fit with substrates, so they don’t work correctly.
Each enzyme has an ideal temperature and pH:
pH: Enzymes are sensitive to acidity and alkalinity. They don’t work properly if an environment is too acidic or basic. For example, an enzyme in the stomach called pepsin breaks down proteins. If your stomach doesn’t have enough acid, pepsin can’t function optimally.
Temperature: Enzymes work best when your body temperature is normal, about 98.6°F (37°C). As temperature increases, enzyme reactions increase. But if the temperature gets too high, the enzyme stops working. That’s why a high fever can disrupt bodily functions.
COMMON CONDITIONS & DISORDERS
What health conditions can enzyme problems cause?
Metabolic disorders are often the result of not having enough of a certain enzyme. Parents can pass them to their children through genes (inherited). Some examples of inherited metabolic disorders include:
Fabry disease prevents body from making enzymes (alpha-galactosidase A) that break down fat (lipids).
Krabbe disease (globoid cell leukodystrophy) affects enzymes needed for the protective covering (myelin) on nerve cells (Central Nervous System).
Maple syrup urine disease affects enzymes needed to break down certain branch chain amino acids.
Other health conditions related to enzyme imbalances include:
Crohn’s disease an imbalance of the bacteria in your gut (gut microbiome) may influence an autoimmune response of the intestinal tract. This may play a role in presentation and severity of Crohn’s disease.
Exocrine pancreatic insufficiency (EPI) is a condition where your pancreas doesn’t have enough digestive enzymes. You can’t break down food or absorb nutrients. Chronic pancreatitis, pancreatic cancer, diabetes or cystic fibrosis can lead to EPI.
Lactose intolerance is a shortage of the enzyme needed to digest sugars in milk (lactose) and dairy.
Apoenzyme
a protein that forms an active enzyme system by combination with a coenzyme and determines the specificity of this system for a substrate
Lecture 12 Transcript
BIOSENSORS
In the field of medicine, industry, agriculture, environment monitoring and biotechnology research, routine analyses using physical instruments are conducted for estimation and monitoring the levels of certain analytes. Conventional physical methods for this routine analysis do not involve the use of any living organisms or molecules of biological origin. However, for this purpose, biological molecules or living cells have been used to develop sensitive devices that are described as ‘biosensors’. The biosensors have been considered to be superior in comparison to physical instruments due to following reasons:
- In a biosensor, immobilized biological material is present in intimate contact of a suitable transducer, so that the biochemical signal is quickly converted into an electrical signal.
- The immobilization of biomolecules permits the reuse of these molecules and allows simplification of the entire apparatus.
iii. The sensing element is present in a small area and is very sensitive, thus facilitating the analysis of substances in very small quantities.
Biosensors provide a useful means for measuring a wide spectrum of analytes (e.g., gases, ions and organic compounds, or even bacteria) and are suitable for studies of complex microbial environments.
What is a biosensor?
A biosensor is an analytical device for the detection of an analyte that combines a biological component with a physicochemical detector component. It consists of 2 parts:
- The sensitive biological element (biological material) (e.g. tissue, microorganisms, organelles, cell receptors, enzymes, antibodies, nucleic acids etc.). The sensitive elements can be created by biological engineering.
- the transducer or the detector element that transforms the signal resulting from the interaction of the analyte with the biological element into another signal (i.e., transducers) that can be more easily measured and quantified.
It detects, records and transmits information regarding a physiological change or the presence of various chemical or biological materials in the environment. An analyte can be a protein, toxin, sugar, antibiotic or vitamin present in the body fluid.
Biosensor is a combination of two parts:
- Bio-element- This part is also known as bioreceptor, biocatalyst or biological active material. It can be an enzyme, antibody, organelle, hormones, nucleic acids or whole cells.
- Sensor-element- This part is also known as transducer. It can be carbon electrode, oxygen electrode, an ion-sensitive electrode, a photocell or a thermistor.
Biosensors were first developed by Clark (Father of Biosensors) in 1962.
The history of biosensors started in the year 1962 with the development of enzyme electrodes by the scientist Leland C. Clark. He used platinum (Pt) electrodes to detect oxygen. The enzyme glucoseoxidase(GOD) was placed very close to the surface of platinum by physically trapping it against theelectrodes with a piece of dialysis membrane. The enzyme activity changes depending on the surrounding oxygen concentration. Glucose reacts withglucose oxidase (GOD) to form gluconic acid while producing two electrons and two protons, thus reducing GOD. The reduced GOD, surrounding oxygen, electrons and protons (produced above) react to form hydrogen peroxide and oxidized GOD (the original form). This GOD can again react with more glucose. The higher the glucose content, more oxygen is consumed. On the other hand, lower glucose content results in more hydrogen peroxide. Hence, either the consumption of oxygen or the production of hydrogen peroxide can be detected by the help of platinum electrodes and this can serve as a measure for glucose concentration.
How do we know there was a detection
If bio-element is specific for the analyte present in the sample, then analyte will bind to the bio-element. Recognition will take place and signal will be produced. If bio-element is not specific for the analyte present in sample, then analyte will not bind to the bio-element. There will be no recognition and signal will not be produced.
Characteristics of Biosensor
- Selectivity is probably the most important feature of a biosensor. Selectivity means that sensor detects a certain analyte and doesn’t react to admixtures and contaminants. Antigen-antibody interaction has the highest selectivity, it is analyte-specific.
- Precision is usually characterised in terms of the standard deviation of measurements. Precision is a characteristic of any scientific device that makes quantitative measurements. If biosensor is not accurate, then there will be fluctuations in the measurements.
- Signal stability shows the signal drift under constant conditions which causes an error in measured concentration. Signal stability influences the precision of sensor. It is animportant characteristic of a sensor that performs continuous monitoring. Signal drift is usually measured in percent per hour.
- Sensitivity (detection limit) shows the minimal amount (or concentration) of analyte that can be detected.
- Working range is the range of analyte concentrations in which the sensor can operate. Working range of sensor should correlate with the range of possible concentrations analyte in the assay. For example, glucose concentration in blood typically varies from 0.2mM to 20 mM. Working range of glucose sensors shouldn’t be less.
- Linear range is the range of analyte concentrations in which the sensor response changes linearly with the concentration.
- Response time is time required to analyze the assay.
- Regeneration time is the time required to return the sensor to working state after interaction with the sample.
- Number of cycles is the number of times the sensor can be operated. Degradation of biological material is inevitable and it needs to be replaced. In some sensors (e.g. hand-held commercial glucose sensors) transducers are disposable, they need to be changed after each measurement. Other sensors can keep their characteristics for many cycles.
- Reproducibility is the accuracy with which sensor’s output can be obtained.
- Life time is the time period over which sensor can be used without significant deterioration in performance characteristics.
- Biosensor should be independent of temperature and pH.
- Biosensors should be economical.
- The complete biosensor should be cheap, small, portable and capable of being used by semi-skilled operators.
Principle of Biosensors
The principle of the biosensor is quite simple. The biological material (enzymes) is firstly immobilized on the immobilization support. Then the sample is passed through the membrane so that analyte present in the sample can react with the immobilized material. After interaction, a biological signal will be produced. This biological signal is then converted by sensor element into electrical signal.
- Bio receptor: An analyte present in the sample would bind to this component only. But it should be highly specific. e.g., glucose oxidase acts only on glucose to produce gluconic acid and hydrogen peroxide. Bio receptor should be stable under storage conditions and it should be immobilized.
- Transducer: acts as an interface since it is present between first and third component. It measures the physical change that occurs with the reaction at the bio receptor
- then transforming that energy into measurable electrical output
Product Sensor
Heat Thermistor
Light Optical transducer
Mass Piezo-electric transducer
current Electrochemical transducer
- Signals from the transducer are passed to a microprocessor where they are amplified and analyzed. The data is then converted to concentration units and transferred to a display or/and data storage device
Lecture 13 Transcript
The MOSFET
(Metal Oxide Semiconductor Field Effect Transistor) transistor is a semiconductor device that is widely used for switching purposes and for the amplification of electronic signals in electronic devices. A MOSFET is either a core or integrated circuit where it is designed and fabricated in a single chip because the device is available in very small sizes. The introduction of the MOSFET device has brought a change in the domain of switching in electronics.
Immunosensors
Description
Immunosensors act on the principle that the immune response of certain biological species (usually bacteria) to contaminants will produce antibodies, which in turn can be measured. To reduce the cost and time required for the accurate analysis of field samples of water and soil contaminated with explosive compounds, such as trinitrotoluene (TNT) and Royal Demolition Explosive (RDX), two immunosensors were developed. They are the fiber-optic biosensor and the continuous flow immunosensor for on-site screening and monitoring of contaminants. Both sensors determine the level of contamination by measuring the level of fluorescent activity caused by the introduction of a biological sample to the system. The fiber-optic biosensor works when contaminant molecules compete with fluorescent antibodies on the sensor. A decrease in fluorescent activity caused by contaminants binding onto antibody sites corresponds to the level of contamination. The continuous flow immunosensor works when the contaminant molecules displace fluorescent antibodies that are placed on a solid support. When displaced antibodies are detected, they correspond proportionally to the level of contamination.
Limitations and Concerns
Methods using biosensors based on fluorescence immunoassay techniques to detect TNT and RDX had a large number of false positive values for the TNT assay.
Insufficient information is presented about these technologies to address fully limitations and concerns.
It is unclear whether these sensors are effective in detecting compounds other than RDX and TNT.
While the sensors can be applied to the screening of chemicals, it is not clear how they would be employed for monitoring. It appears that the contaminant must come into direct contact with the sensor. More information is needed on how the sensors can be arranged to serve a monitoring function.
Applicability
These sensors are analytical tools to detect TNT and RDX in soil and groundwater. Both sensors are portable, quick (2–10 minutes per analysis), and sensitive (low parts-per-billion concentration detection).
Technology Development Status
The fiber-optic biosensor and the continuous flow immunosensor, developed at the Naval Research Laboratory (NRL) in collaboration with Research International, will be employed at a site for the detection of TNT and RDX. These sensors are considered pilot projects.
Lecture 14 Transcript
What is a smart sensor?
A smart sensor is a device that takes input from the physical environment and uses built-in compute resources to perform predefined functions upon detection of specific input and then process data before passing it on.
Smart sensors enable more accurate and automated collection of environmental data with less erroneous noise amongst the accurately recorded information. These devices are used for monitoring and control mechanisms in a wide variety of environments including smart grids, battlefield reconnaissance, exploration and many science applications.
The smart sensor is also a crucial and integral element in the internet of things (IoT), the increasingly prevalent environment in which almost anything imaginable can be outfitted with a unique identifier and the ability to transmit data over the internet or a similar network. One implementation of smart sensors is as components of a wireless sensor and actuator network (WSAN) whose nodes can number in the thousands, each of which is connected with one or more other sensors and sensor hubs, as well as individual actuators.
Compute resources are typically provided by low-power mobile microprocessors. At a minimum, a smart sensor is made of a sensor, a microprocessor and communication technology of some kind. The compute resources must be an integral part of the physical design — a sensor that just sends its data along for remote processing isn’t considered a smart sensor.
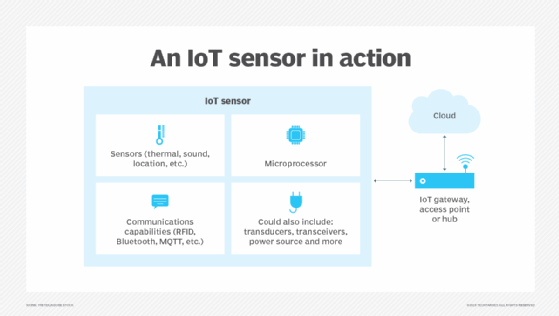
A smart sensor has three components: a sensor that captures data, a microprocessor that computes on the output of the sensor via programming and communications capabilities.
A smart sensor might also include several other components besides the primary sensor. These components can include transducers, amplifiers, excitation control, analog filters and compensation. A smart sensor also incorporates software-defined elements that provide functions such as data conversion, digital processing and communication to external devices.
How do smart sensors work?
A smart sensor ties a raw base sensor to integrated computing resources that enable the sensor’s input to be processed.
The base sensor is the component that provides the sensing capability. It might be designed to sense heat, light or pressure. Often, the base sensor will produce an analog signal that must be processed before it can be used. This is where an intelligent sensor’s integrated technology comes into play. The onboard microprocessor filters out signal noise and converts the sensor’s signal into a usable, digital format.
Smart sensors also contain integrated communications capabilities that enable them to be connected to a private network or to the internet. This enables communication to external devices.
What are smart sensors used for?
There are countless use cases for smart sensors. They are very commonly used in industrial environments and are the driving force behind Industry 4.0.
Factories often use smart temperature sensors to make sure machines aren’t overheating, and vibration sensors to make sure machines aren’t at risk of vibrating loose. Smart sensors also enable process control, such as monitoring a process, like manufacturing an item, and making any adjustments that might be required to meet quality or production goals. This was once a manual process, but smart sensors can be used to automate process control.
Smart sensors also play a key role in modern security systems. Thermal imaging sensors can be used to detect an intruder’s body heat. Similarly, devices such as smart locks, motion sensors, and window and door sensors are commonly connected to a common network. This enables the security sensors to work together to paint a comprehensive picture of the current security status.
What are different types of smart sensors?
There are five main types of smart sensors used in industrial environments. Although there are many types of special purpose sensors in use today, they are generally based on one of five types of sensors.
- Level sensors. A level sensor is used to measure the volume of space taken up in a container. A vehicle’s fuel gauge might be connected to a level sensor that monitors the level of fuel in the tank.
- Temperature sensors. A temperature sensor is a sensor that can monitor a component’s temperature so a corrective action can be taken if necessary. In an industrial setting for example, a temperature sensor can be used to make sure machinery is not overheating.
- Pressure sensor. Pressure sensors are often used to monitor the pressure of gasses or fluids in a pipeline. A sudden drop in pressure might indicate a leak or a flow control issue.
- Infrared sensors. Some infrared sensors, such as those used in thermal imaging cameras or noncontact infrared thermometers are used for temperature monitoring. Other infrared sensors are optical sensors tuned to a frequency that enables them to see light in the infrared spectrum. These types of sensors are used in medical equipment, such as pulse oximetry devices, and in electronic devices designed to be operated by remote control.
- Proximity sensors. A proximity sensor is used to detect the location of a person or object with relation to the sensor. In retail environments, proximity sensors can track customer movements throughout the store.
How are smart sensors different from base sensors?
Smart sensors include an embedded Digital Motion Processor (DMP), whereas base sensors don’t. A DMP is, essentially, just a microprocessor that is integrated into the sensor. It enables the sensor to perform onboard processing of the sensor data. This might mean normalizing the data, filtering noise or performing other types of signal conditioning. In any case, a smart sensor performs data conversion digital processing prior to any communication to external devices.
A base sensor is simply a sensor that isn’t equipped with a DMP or other compute resources that would enable it to process data. Whereas a smart sensor produces output that is ready to use, a base sensor’s output is raw and must typically be converted into a usable format.
Smart sensors are generally preferred over base sensors because they include native processing capabilities. Even so, there are situations where it might be more advantageous to use a base sensor. If an engineer is designing a device and needs complete control over sensor input, then it will probably make more sense to use a base sensor than a smart sensor. Base sensors also cost less than smart sensors because they contain fewer components.
Although smart sensors are most often associated with industrial equipment, IoT couldn’t exist without smart sensors. Learn more about the use cases and benefits of smart sensors for IoT.